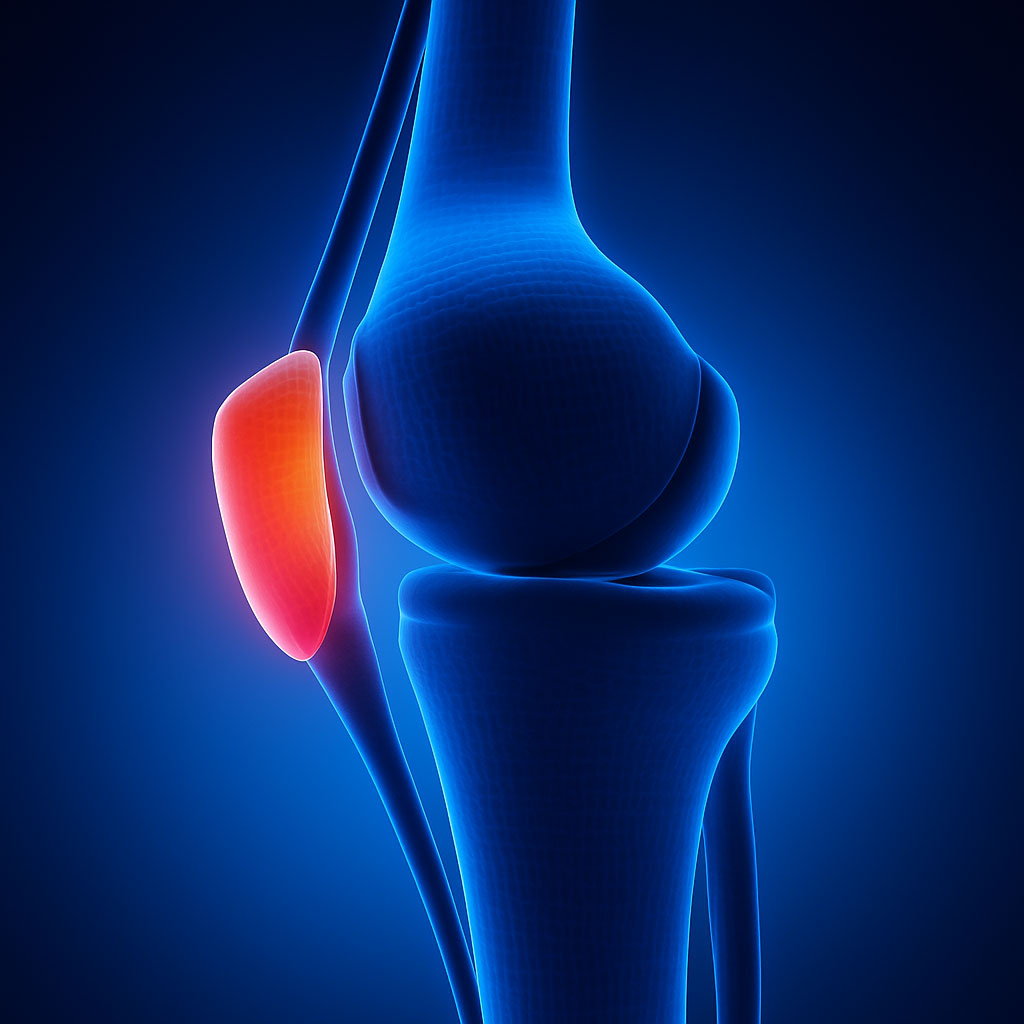
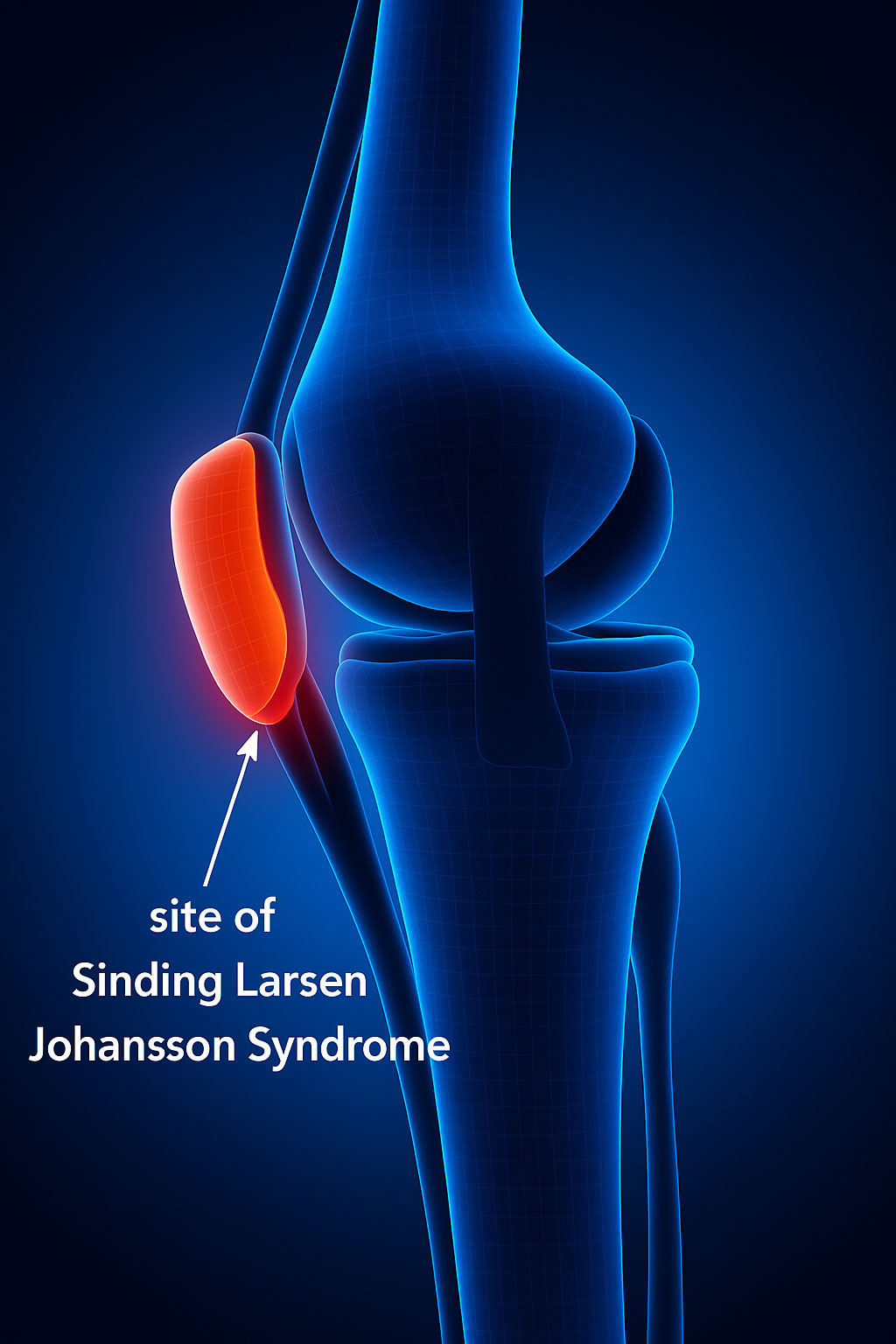
Sinding-Larsen-Johansson disease (SLJ) is a type of osteochondrosis and, like Osgood-Schlatter disease, it is characterized by knee pain.
It is an inflammation of the lower pole of the patella, caused by repetitive stress on the patellar tendon.
Two main forms are recognized:
- Early-onset form: typically appears between the ages of 5 and 7.
- Late-onset form: develops between the ages of 9 and 14, during puberty.
In both cases, bilateral involvement is relatively common. The late-onset form is more frequent in adolescents, particularly in young male athletes, and it is often associated with Osgood-Schlatter disease. Like other osteochondroses, SLJ is thought to result from multiple contributing factors, with repeated microtrauma and the changes it produces playing a central role.
Causes
When a child’s legs begin to straighten, the quadriceps muscle exerts tension on the patellar tendon, placing stress on the growth plate at the lower part of the patella.
During periods of rapid growth, bones lengthen faster than muscles and tendons can adapt. If muscle growth does not keep pace with the lengthening of the femur, the resulting tension increases the load on the patellar tendon and the growth plate.
Sinding-Larsen-Johansson disease most commonly affects children aged 10 to 14 who participate in sports involving frequent jumping or running.
Diagnosis
Symptoms are fairly consistent and may include:
- Localized pain at the front of the knee, especially at the lower pole of the patella
- Swelling around the kneecap
- Pain that worsens with physical activity such as jumping, climbing, running, squatting, or going up and down stairs
- Pain that begins gradually, is intermittent, and often more noticeable with exertion (e.g., descending stairs or sports practice
- Symptoms that may be unilateral or bilateral
- Relief of pain with rest
- Mild limitation of active extension, sometimes accompanied by a slight limp
During the clinical examination, the physician will assess the knee for swelling and tenderness, as well as review the child’s medical history and participation in sports.
Imaging tests, such as X-rays or MRI scans, are rarely necessary but may be recommended to rule out other conditions, including injuries or infections.
Treatment
Treatment typically includes:
- Partial or complete rest from activities that stress the knee
- Application of ice
- Stretching exercises to relieve tension on the tendon
- Instrumental physiotherapy such as laser therapy or tecar therapy
Return to sports should be gradual, and in some cases, the use of patellar straps or braces may be recommended to reduce stress on the tendon.
Prognosis
Recovery is generally complete. Thanks to the young age of affected patients, no lasting functional limitations are expected, and there is no evidence of long-term complications such as early-onset osteoarthritis.
However, it is important to note that symptoms may persist until the bones are fully mature and the patellar growth plate has completely closed.
The Role of the Riva Method
While Sinding-Larsen-Johansson disease typically resolves with rest and conservative management, many young athletes experience recurring symptoms or prolonged recovery times due to inadequate neuromuscular control and repeated overload on the patellar tendon.
The Riva Method offers a valuable complementary approach by focusing on proprioceptive training and postural reprogramming. By improving lower-limb stability, optimizing load distribution, and enhancing the activation of stabilizing muscles, the Riva Method reduces excessive stress on the patellar tendon, promoting a faster and safer return to sports.
In addition to supporting the healing process, the method helps prevent relapses and future overuse injuries, enabling young athletes to regain confidence, restore efficient movement patterns, and protect knee health during growth and athletic development.