What is ankle instability?
Ankle instability is a condition in which patients experience a recurrent sensation of weakness or inability to support their body weight, often accompanied by frequent ankle “giving way” while walking or running. Sometimes this presents as a fleeting sensation, while in other cases it may lead to repeated sprains, worsening instability, or even falls.
The most common underlying cause of chronic ankle instability is an inadequately treated ankle sprain.
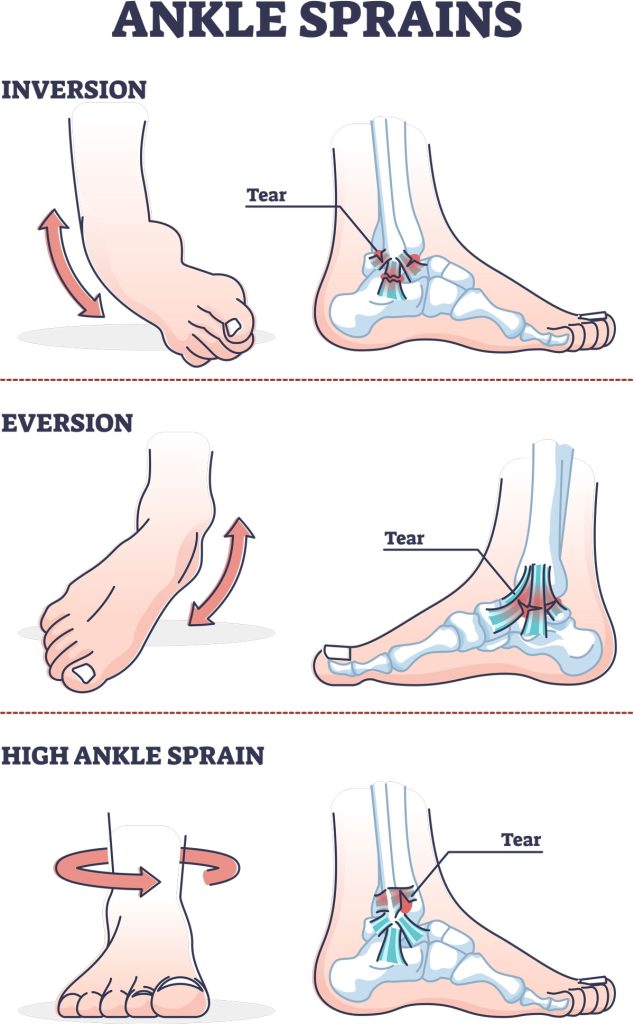
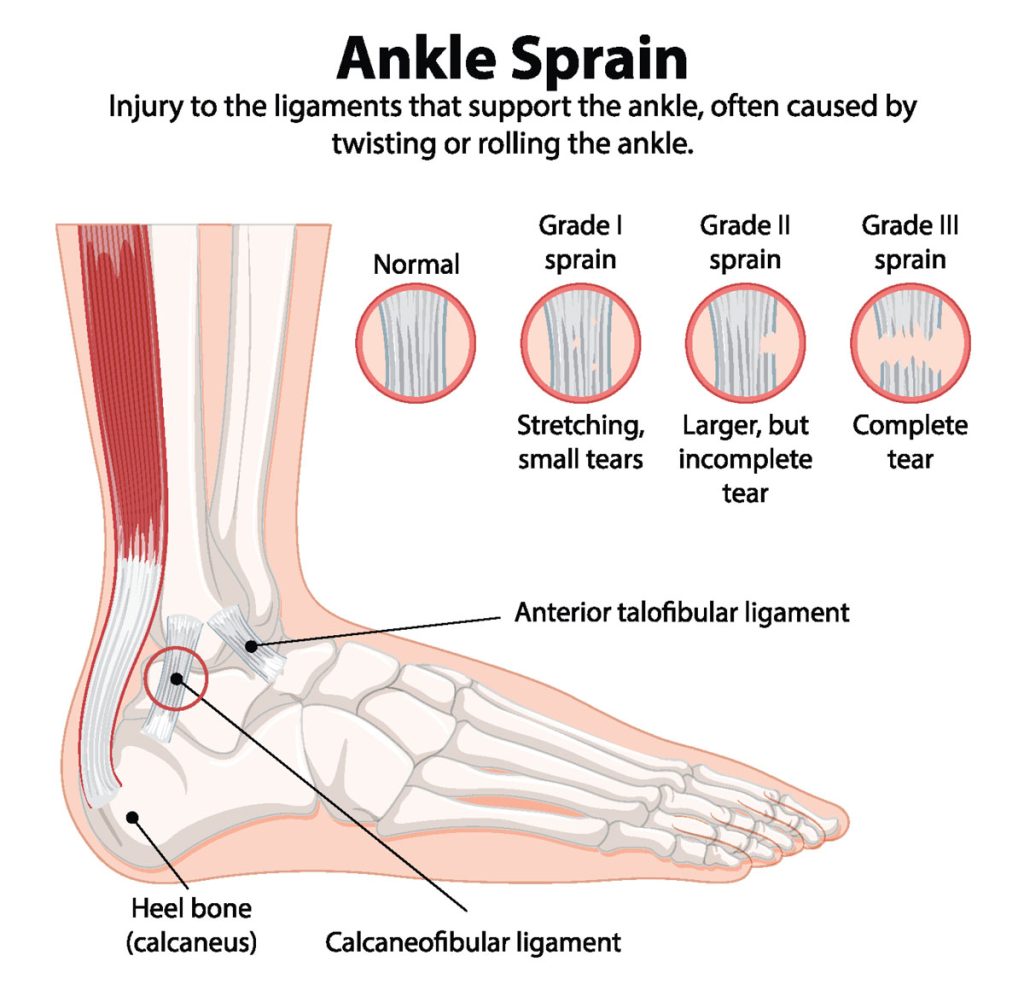
An acute sprain can damage or rupture the ligaments on the outer or inner side of the ankle, or create pathological changes inside the joint. These conditions often coexist, re sulting in what is termed chronic ankle instability.
If left untreated, injured ligaments fail to regain their original tension, stabilizing muscles weaken and cannot effectively perform their role, and the joint remains exposed to recurrent sprains.
Types of chronic ankle instability
Chronic ankle instability is generally classified into two main categories, which usually coexist to varying degrees:
- Anatomical instability: caused by partial or complete ligament injury on the outer or inner side of the ankle.
- Functional instability: caused by inadequate proprioceptive control and weakness of the stabilizing muscles.
In reality, functional instability almost always includes an anatomical component, in the form of ligament laxity (ligaments become stretched and lose their stabilizing function) as a result of previous sprains.
Causes of ankle instability
Although the most frequent cause is a previous ankle sprain with capsulo-ligamentous damage, the deeper origin often lies in modern lifestyle habits. A lack of interaction with uneven terrain, combined with thousands of daily steps only on flat surfaces, leads to progressive weakening of ligaments, joint capsule, muscles, and tendons. These tissues then become more fragile and less effective in responding to unexpected environmental challenges.
Diagnosis
Accurate diagnosis requires imaging studies such as weight-bearing X-rays, ultrasound, CT scan, and especially MRI, which is the most informative tool for assessing not only muscles, tendons, and ligaments, but also the condition of the cartilage.
Treatment of ankle instability
Chronic ankle instability should always be managed with the primary goal of restoring maximum functional stability, even in the presence of ligament damage. Surgery may be considered only later, in carefully selected cases. It is essential for both patients and athletes to understand that surgery cannot replace the proprioceptive retraining needed to restore reflex stabilization mechanisms.
The Riva Method
Scientific studies published internationally have shown that the Riva Method achieves the highest efficacy ever reported, reducing ankle sprains by 81%.
The Riva Method is based on High-Frequency Proprioceptive Training (HFPT), which produces:
- Improved proprioceptive control, leading to:
- better single-leg stance stability through reflex activation,
- increased braking strength of stabilizing muscles against sprains,
- rebalancing of foot alignment in the flight phase before ground contact.
- Greater endurance of proprioceptive control, i.e. the ability to maintain stability even under fatigue.
- Increased resilience of ligaments and joint capsule, enhancing their ability to deform and return to the previous status without damage, absorbing the residual kinetic energy during a sprain.
For this reason, three-quarters of NBA basketball teams use this methodology. NBA athletes who train with the Riva Method and the Delos system report that sprain-like events, which would previously have caused injury, are now absorbed without damage.
Surgical treatment
Surgery is considered only in severe cases where, after at least four months of high-frequency and high-density proprioceptive training (HFPT + HHPT) following the Riva Method, significant instability persists, impairing daily life or sports activity.
It is crucial to allow at least four months of intensive HHPT, so that muscular and ligamentous adaptations have the necessary biological time to become effective.