We recommend reading the story of a basketball player who experienced this severe injury (Lisfranc fracture-dislocation).
What is it?
A Lisfranc injury is a fracture and/or dislocation of the midfoot that involves one or more joints of the tarsometatarsal (TMT) region. Fractures of the Lisfranc joint complex are rare—about 1% of all fractures. However, this number is likely underestimated, since many midfoot injuries go unrecognized and patients may only seek specialist evaluation years after the trauma.
The Lisfranc joint complex is made up of the five TMT joints that connect the forefoot and the metatarsals. Several ligaments stabilize this complex. The Lisfranc ligament, in particular, connects the base of the second metatarsal to the medial cuneiform. Lisfranc injuries can vary widely in severity—from a simple sprain to a dislocation of one or more TMT joints, with or without fractures. When fractures occur, they often involve the second metatarsal. These injuries frequently lead to midfoot instability.
Causes of Lisfranc Injury
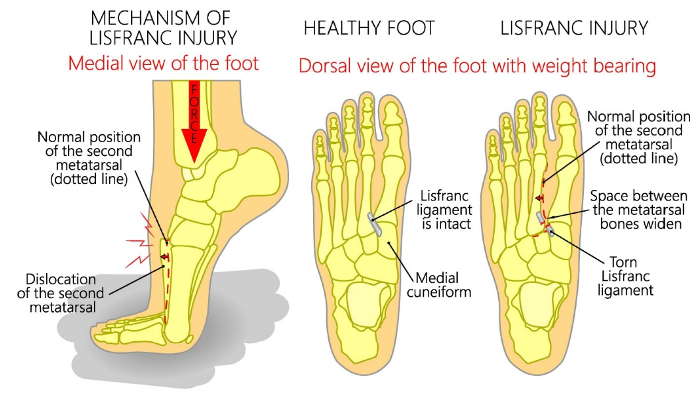
Lisfranc dislocations usually result from high-energy trauma, such as motor vehicle or motorcycle accidents, falls from height, or sports injuries. They can also occur from lower-energy trauma, often involving an indirect twisting force applied to a foot in plantarflexion. A classic example is when a rider falls from a horse and the foot remains trapped in the stirrup. Historically, this type of injury was common on battlefields during cavalry charges and was first described by Jacques Lisfranc, Napoleon’s surgeon.

In high-energy trauma, forces are typically direct, and fractures are often associated with dislocations. For this reason, the term Lisfranc fracture-dislocation is commonly used, describing a midfoot fracture combined with complex ligamentous injury.
Diagnosis
The severity of Lisfranc injuries can vary greatly. Some cause only mild swelling and pain in the middle of the foot, while others result in severe soft tissue pain, marked swelling, deformity, bruising on the sole, and sometimes numbness or tingling. The foot may even appear shortened. Total dislocations are usually easy to diagnose, but minimal dislocations can be much harder to detect.
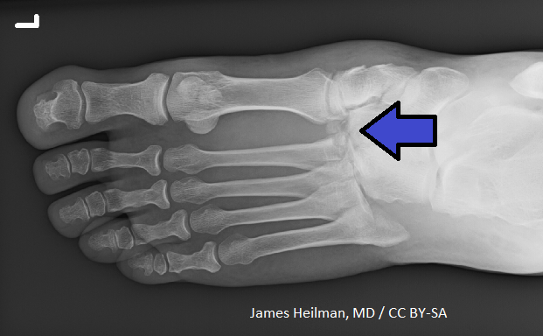
In uncertain cases, additional imaging is essential. CT scans are particularly useful, but when not available, stress radiographs can help—such as taking X-rays while the patient stands on one foot. Bearing weight may reveal a gap between the first and second metatarsals, making diagnosis easier. CT remains more sensitive than stress radiography.
Unfortunately, Lisfranc dislocations are often missed and mistaken for simple sprains. When left untreated, they frequently progress to further dislocation under load, leading to deformities and, almost inevitably, arthritic changes over time.
Surgical Treatment
Midfoot injuries often require surgery. The standard approach is open reduction and internal fixation (ORIF), in which bones are repositioned and held in place using wires, screws, or plates. These implants remain until the bones or joints have healed, and are often removed later with a second procedure.
In more severe cases, fusion (arthrodesis) may be recommended. This involves surgically fusing damaged bones together so they heal as a single, stable unit.
The Riva Method Approach
When discussing causes of Lisfranc injuries, structural characteristics of the foot are often overlooked as contributing factors. However, it is increasingly clear that lifestyle in developed countries leads to progressive structural and functional deterioration of the feet. This results in significant fragility of muscles, ligaments, tendons, capsules, and even bones.
Among young people, the situation is often worse: the natural maturation process of the foot has remained incomplete, both anatomically and functionally. This has short-, medium-, and long-term consequences throughout the body—for example, recurring lower back pain.
The Riva Method can play a preventive role by counteracting these deficits. By improving single-leg stance stability through proprioceptive control, and by promoting structural remodeling with high-frequency proprioceptive training (HPT), it protects the foot by:
- Minimizing the mechanical stress generated with each ground impact that otherwise loads the midfoot.
- Increasing the structural resilience of the foot, improving its tolerance to both repetitive and impact-related mechanical stress.
Rehabilitation After Lisfranc Injury
Whether treated surgically or not, depending on severity, the Riva Method can significantly improve functional recovery. A Lisfranc injury is devastating to the architecture of the midfoot, and surgery alone cannot restore the foot’s complex anatomical and functional role as the body’s interface with the ground.
The Riva Method can be initiated once weight-bearing is possible, beginning with bilateral loading and progressing to single-leg exercises. Using the Delos system, hundreds of thousands of stimulations can be applied to help restore the foot’s load-bearing capacity. This process induces true structural remodeling—affecting muscles, tendons, ligaments, joint capsules, and bones.
A structured program of 3 to 6 months is typically required to achieve results that would otherwise be unattainable. Noticeable improvements usually begin within the first few weeks and continue to grow over time.
We recommend reading the story of a basketball player who suffered this serious injury (Lisfranc fracture-dislocation).


